When Is My Limb Threatened in Peripheral Artery Disease (PAD)?
Peripheral artery disease (PAD) is a condition in which the arteries that carry blood to your legs and feet become narrowed or blocked by cholesterol plaque. Many people think of PAD only as a “leg problem,” but in reality it is a sign of widespread vascular disease that also raises the risk of heart attack and stroke.
A common question patients ask is: “When is my limb actually threatened?”
The answer depends on where you are along the spectrum of PAD.
Understanding this spectrum can help you recognize danger early—and get care before permanent damage occurs.
Stage 1: No Symptoms (Silent PAD)
Many people with PAD feel perfectly normal at first. Their circulation is reduced, but not enough to cause pain.
Even in this early stage, risk is real. People with PAD—even without symptoms—are more likely to suffer:
Heart attack
Stroke
Worsening leg circulation over time
This is why doctors often recommend:
Cholesterol medicine
Blood pressure control
Aspirin (in selected patients)
Smoking cessation
Regular walking
At this stage, your limb is not yet threatened, but your overall cardiovascular health is.
Stage 2: Intermittent Claudication (Pain With Walking)
As blockages worsen, people may develop intermittent claudication—cramping, aching, or tightness in the calf, thigh, or buttock when walking that improves with rest.
This is a warning sign that blood flow is limited.
At this stage:
Your limb is not immediately threatened, but you are at higher risk of progression
You are also at significantly higher risk of heart attack and stroke compared with people without PAD
Many patients can improve with:
Supervised walking programs
Medications to improve circulation
Aggressive risk-factor control
Some may need procedures if symptoms severely limit their daily life.
Stage 3: Rest Pain — Your Limb Is Now in Danger
When PAD becomes severe, blood flow may be so poor that you feel pain in your feet even while resting, especially at night.
People often describe this as:
Burning pain in the toes or forefoot
Pain that improves when they dangle their leg off the bed
Pain that wakes them from sleep
This is a critical turning point.
👉 Rest pain means your limb is threatened.
Patients with rest pain should be evaluated urgently by a vascular specialist, because the risk of tissue damage and amputation rises quickly.
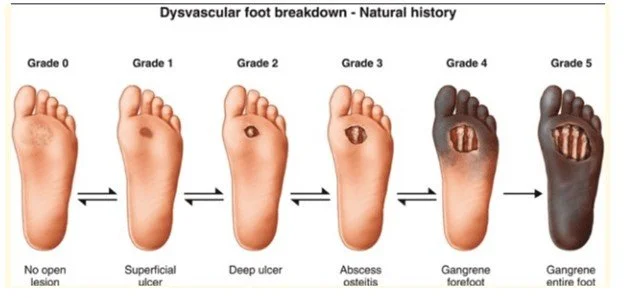
Stage 4: Tissue Loss — This Is a Limb Emergency
The most advanced and dangerous stage of PAD is tissue loss, which includes:
A foot ulcer that will not heal
Black or dead skin (gangrene)
Deep infection in the foot
Exposed bone or tendon
At this stage:
The limb is severely threatened
The risk of amputation is high
The risk of heart attack and stroke is also very high
This is not a “wait and see” situation.
Patients with tissue loss should be seen as soon as possible—ideally within days—by a limb salvage team.
Why PAD Is More Than a Leg Problem
At every stage of PAD—mild or severe—patients are at higher risk for:
Heart attack
Stroke
Kidney disease
Worsening circulation in the legs
That is why treatment must focus on the whole person, not just the leg:
Heart health
Blood pressure
Cholesterol
Diabetes control
Smoking cessation
Saving the limb often goes hand in hand with saving the life.
Why Multispecialty Care Matters
The best outcomes for threatened limbs come from team-based care, not one doctor working alone.
A strong limb salvage program typically includes:
Vascular surgery
Podiatry (foot specialists)
Wound care nurses
Infectious disease specialists
Endocrinology (diabetes care)
Cardiology
Primary care
Physical therapy and rehabilitation
This team works together to:
Restore blood flow when possible
Heal wounds
Prevent infection
Optimize heart and kidney health
Help patients regain mobility and independence
Research consistently shows that patients treated in coordinated limb salvage programs have fewer amputations, faster healing, and better survival.
A Final Message of Hope
PAD is serious—but it is also treatable.
Claudication can often be improved
Rest pain can frequently be relieved with timely treatment
Even many patients with ulcers can avoid amputation when treated quickly and properly
If you have PAD—or think you might—don’t wait for a crisis. Early recognition and coordinated care can protect your legs, your heart, and your future.
Below is a clear, practical, patient-friendly checklist you can place at the end of your blog, use as a clinic handout, or share at community events. It mirrors the stages in your blog and emphasizes urgency, whole-person risk, and team care.
Is My Limb Threatened? — PAD Patient Checklist
Use this checklist to understand your risk, recognize danger early, and know when to seek care.
✅ 1) Do I have risk factors for PAD? (Check all that apply)
☐ Age 50 or older
☐ Current or past smoker
☐ Diabetes
☐ High blood pressure
☐ High cholesterol
☐ Kidney disease
☐ Heart disease or prior heart attack
☐ Prior stroke or TIA (“mini-stroke”)
☐ Little physical activity
☐ Family history of vascular disease
👉 If you checked 1 or more boxes: ask your doctor about PAD screening (ABI test).
✅ 2) Do I have symptoms with walking? (Claudication stage)
☐ Cramping, aching, or tightness in calf, thigh, or buttock when walking
☐ Pain that goes away with rest
☐ Slower walking speed or shorter walking distance than before
👉 What this means:
Your limb is not yet in immediate danger, but your risk for worsening disease, heart attack, and stroke is higher than average.
Ask your clinician about:
☐ ABI test
☐ Walking program
☐ Cholesterol and blood pressure medicines
✅ 3) Do I have rest pain? — THIS IS URGENT
☐ Burning pain in toes or forefoot while resting
☐ Pain that wakes me up at night
☐ Pain that feels better when I dangle my leg off the bed
👉 What this means:
Your limb is threatened.
You should be seen urgently by a vascular specialist.
Ask for:
☐ Urgent vascular evaluation
☐ Circulation testing
☐ Possible revascularization plan
✅ 4) Do I have tissue loss? — THIS IS A LIMB EMERGENCY
☐ Open sore or ulcer on foot or toes that won’t heal
☐ Black or dead skin (gangrene)
☐ Spreading redness, warmth, or foul drainage
☐ Fever or feeling sick
☐ Deep wound with visible tissue
👉 Do NOT wait.
Seek care as soon as possible and request a multispecialty limb salvage team.
✅ 5) Am I protecting my heart and brain too?
If you have PAD at any stage, ask your doctor about:
☐ Cholesterol medicine (statin)
☐ Blood pressure control
☐ Aspirin or other antiplatelet (if appropriate)
☐ Diabetes control plan
☐ Smoking cessation support
☐ Regular walking program
Remember: PAD is a warning sign for heart attack and stroke.
✅ 6) Have I been connected to a team?
Optimal care usually involves more than one specialist:
☐ Vascular surgery
☐ Podiatry (foot care)
☐ Wound care
☐ Diabetes specialist
☐ Cardiology
☐ Primary care
☐ Physical therapy / rehab
Ask:
“Can I be referred to a limb salvage program?”
🚨 When to seek care immediately
Go to urgent care or the ER if you have:
New rest pain in the foot
Any foot ulcer with redness, swelling, or drainage
Black tissue or gangrene
Fever or feeling very sick with a foot wound
Bottom line for patients
Claudication = warning sign
Rest pain = limb is threatened
Tissue loss = limb emergency
Early action + team care can often save your limb and protect your life.
If you want, I can:
Turn this into a one-page printable PDF,
Make a graphic checklist or poster, or
Brand it for a Cleveland Clinic blog or community handout.